Difference between revisions of "Germ cell tumours"
Jump to navigation
Jump to search

(change term ITGCN --> GCNIS) |
|||
| Line 62: | Line 62: | ||
! Image | ! Image | ||
|- | |- | ||
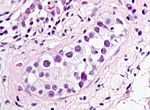
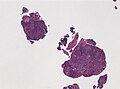
| [[ | | [[Germ cell neoplasia in situ]] (GCNIS) | ||
| nests of small fried egg cells | | nests of small fried egg cells | ||
| large central nucleus, clear <br>cytoplasm, squared-off nuclear membrane, nucleoli<ref name=Ref_GUP538>{{Ref GUP|538}}</ref> | | large central nucleus, clear <br>cytoplasm, squared-off nuclear membrane, nucleoli<ref name=Ref_GUP538>{{Ref GUP|538}}</ref> | ||
| CD117 +ve, CD30 -ve | | CD117 +ve, CD30 -ve | ||
| appearance similar to [[seminoma]] | | appearance similar to [[seminoma]] | ||
| [[Image:Intratubular_germ_cell_neoplasia_high_mag_cropped.jpg|thumb|center|150px| | | [[Image:Intratubular_germ_cell_neoplasia_high_mag_cropped.jpg|thumb|center|150px|GCNIS (WC/Nephron)]] | ||
|- | |- | ||
| [[Germinoma]] / [[Seminoma]] / [[Dysgerminoma]] | | [[Germinoma]] / [[Seminoma]] / [[Dysgerminoma]] | ||
Revision as of 23:25, 15 March 2016

Testicular mixed germ cell tumour. (WC/euthman)
This article covers germ cell tumours, often abbreviated GCT, which classically arise in the gonads (ovary, testis). They are also found in the midline and make appearances in neuropathology (e.g. pineal gland) and in the mediastinum.
Overview
Germ cell tumour - types
Precusor:
Germ cell tumours (GCTs):
- Germinoma/Seminoma/Dysgerminoma.
- Yolk sac tumour (endodermal sinus tumour).
- Embryonal carcinoma.
- Choriocarcinoma.
- Teratoma.
- Mixed germ cell tumour (mixed GCT) - 60% of GCTs are mixed.
- Common combinations:
- teratoma + embryonal carcinoma + endodermal sinus tumour (yolk sac tumour) (TEE).
- seminoma + embryonal (SE).
- embryonal + teratoma (TE).
- Common combinations:
- Gonadoblastoma.
- Polyembryoma.
Grossing
Main article: Orchiectomy
- 1 cm2 of tumour per cm of maximal tumour dimension - guideline for testicular cancer.[1]
IHC for GCTs
ISUP
An algorithmic approach based on the ISUP consensus paper by Ulbright et al.:[2]
| Germ cell tumours | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| OCT4 +ve | OCT4 -ve | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
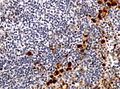
| CD117 +ve CD30 -ve | CD117 -ve CD30 +ve | Glypican 3 +ve AFP +ve beta-hCG -ve | Glypican 3 ? AFP -ve beta-hCG +ve | Glypican 3 -ve AFP -ve beta-hCG -ve | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Seminoma | Embryonal carcinoma | Yolk sac tumour | Choriocarcinoma | Spermatocytic seminoma | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
ABCDs of GCTs
- AFP - yolk sac tumour.
- Beta-hCG - choriocarcinoma.
- CD30 - embryonal carcinoma.
- D2-40 - seminoma.
GCT versus sex cord-stromal tumour
The ISUP recommends:[3]
Alternates for SALL4 are:[3]
- OCT4 and GPC3.
Tabular summary of GCTs
| Tumour | Key feature | Microscopic | IHC | Other | Image |
|---|---|---|---|---|---|
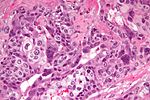
| Germ cell neoplasia in situ (GCNIS) | nests of small fried egg cells | large central nucleus, clear cytoplasm, squared-off nuclear membrane, nucleoli[5] |
CD117 +ve, CD30 -ve | appearance similar to seminoma | |
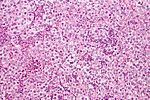
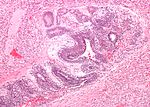
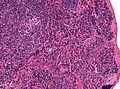
| Germinoma / Seminoma / Dysgerminoma | fried egg cells | fried egg-like cells (central nucleus, clear cytoplasm) with squared-off nuclear membrane, nucleoli, lymphocytic infiltrate, granulomata, syncytiotrophoblastic giant cells[6] |
D2-40 | seminoma = male version of this tumour; dysgerminoma = female version of this tumour | |
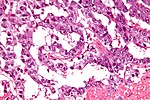
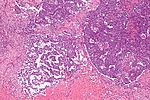
| Yolk sac tumour (endodermal sinus tumour) | Schiller-Duval bodies | Schiller-Duval b. = central blood vessel surrounded by epithelial-like cells a space and more epithelial-like cells, variable arch. | AFP +ve, Glypican 3 +ve | patterns: microcystic, solid, hepatoid | |
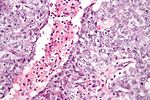
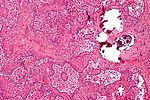
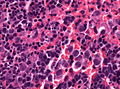
| Embryonal carcinoma | prominent nucleoli, vescicular nuclei | var. arch.: tubulopapillary, glandular, solid, embryoid bodies (ball of cells in surrounded by empty space on three sides), +/-nuclear overlap, mitoses common | CD30 +ve, CD117 -ve | usu. part of a mixed GCT | |
| Choriocarcinoma | clear cytoplasm | cells with abundant clear cytoplasm and eccentric atypical nuclei (cytotrophoblast), very large (multinucleated) cells with abundant eosinophilic cytoplasm and extreme nuclear atypia (syncytiotrophoblast) | beta-hCG +ve | may be preceded by a complete hydatidiform mole | |
| Teratoma, immature | primitive neuroepithelium | pseudostratified epithelium in rosettes (gland-like arrangement) | None | testicular teratomas in post-pubertal males are all considered malignant[7] | |
| Mixed germ cell tumour | NA | common combinations: teratoma + embryonal carcinoma + endodermal sinus tumour (yolk sac tumour) (TEE); seminoma + embryonal (SE); embryonal + teratoma (TE) | NA | - | |
| Gonadoblastoma | primitive germ cells (central nucleus, moderate (eosinophilic) cytoplasm); sex cord element | sex cord element may be either granulosa cells (follicle-like arch.) or Sertoli cells (trabecular arch.) | ? | often abnormal karyotype; usu. Y chromosome present |
Molecular pathology
Most common cytogenetic abnormality in GCTs:
- Isochromosome p12.[8]
- Isochromosome = one arm (p or q) is lost and replaced with a duplicate of the remaining one.
- Example: isochromosome p12 = chromosome 12 where q is lost and two p arms are present.[9]
- Isochromosome = one arm (p or q) is lost and replaced with a duplicate of the remaining one.
Germinoma
Comes in three flavours:
- Germinoma.
- Seminoma.
- Dysgerminoma.
Germinoma
Is the generic version of this tumour. It is found in the midline (brain, mediastinum).
Image: Germinoma (upmc.edu).[10]
Seminoma
Main article: Seminoma
A common GCT in males.
Dysgerminoma
Main article: Ovarian tumours#Dysgerminoma
A common GCT in females.
Yolk sac tumour
Main article: Yolk sac tumour
Embryonal carcinoma
Main article: Embryonal carcinoma
Choriocarcinoma
Main article: Choriocarcinoma
Teratoma
Main article: Teratoma
Gonadoblastoma
Main article: Gonadoblastoma
Polyembryoma
Main article: Polyembryoma
Mixed germ cell tumour
Main article: Mixed germ cell tumour
See also
References
- ↑ URL: http://www.uroweb.org/gls/pdf/10_Testicular_Cancer.pdf. Accessed on: 30 October 2012.
- ↑ Ulbright TM, Tickoo SK, Berney DM, Srigley JR (August 2014). "Best practices recommendations in the application of immunohistochemistry in testicular tumors: report from the international society of urological pathology consensus conference". Am. J. Surg. Pathol. 38 (8): e50–9. doi:10.1097/PAS.0000000000000233. PMID 24832161.
- ↑ 3.0 3.1 Amin MB, Epstein JI, Ulbright TM, et al. (August 2014). "Best practices recommendations in the application of immunohistochemistry in urologic pathology: report from the international society of urological pathology consensus conference". Am. J. Surg. Pathol. 38 (8): 1017–22. doi:10.1097/PAS.0000000000000254. PMID 25025364.
- ↑ Miettinen M, Wang Z, McCue PA, et al. (March 2014). "SALL4 expression in germ cell and non-germ cell tumors: a systematic immunohistochemical study of 3215 cases". Am. J. Surg. Pathol. 38 (3): 410–20. doi:10.1097/PAS.0000000000000116. PMID 24525512.
- ↑ Zhou, Ming; Magi-Galluzzi, Cristina (2006). Genitourinary Pathology: A Volume in Foundations in Diagnostic Pathology Series (1st ed.). Churchill Livingstone. pp. 538. ISBN 978-0443066771.
- ↑ Zhou, Ming; Magi-Galluzzi, Cristina (2006). Genitourinary Pathology: A Volume in Foundations in Diagnostic Pathology Series (1st ed.). Churchill Livingstone. pp. 542. ISBN 978-0443066771.
- ↑ Carver, BS.; Al-Ahmadie, H.; Sheinfeld, J. (May 2007). "Adult and pediatric testicular teratoma.". Urol Clin North Am 34 (2): 245-51; abstract x. doi:10.1016/j.ucl.2007.02.013. PMID 17484929.
- ↑ Looijenga, LH.; Oosterhuis, JW. (May 1999). "Pathogenesis of testicular germ cell tumours.". Rev Reprod 4 (2): 90-100. PMID 10357096.
- ↑ URL: http://ghr.nlm.nih.gov/handbook/illustrations/isochromosomes. Accessed on: 15 February 2012.
- ↑ URL: http://path.upmc.edu/cases/case525.html. Accessed on: 25 January 2012.