Difference between revisions of "Germ cell tumours"
| Line 412: | Line 412: | ||
Image:Strumal_carcinoid_-_high_mag.jpg | Strumal carcinoid - high mag. (WC/Nephron) | Image:Strumal_carcinoid_-_high_mag.jpg | Strumal carcinoid - high mag. (WC/Nephron) | ||
</gallery> | </gallery> | ||
===Sign out=== | |||
====Mature teratoma==== | |||
<pre> | |||
CYST ("DERMOID"), RIGHT OVARY, CYSTECTOMY: | |||
- MATURE CYSTIC TERATOMA. | |||
</pre> | |||
==Gonadoblastoma== | ==Gonadoblastoma== | ||
===General=== | ===General=== | ||
Revision as of 18:07, 24 May 2013
This article covers germ cell tumours, often abbreviated GCT, which classically arise in the gonads (ovary, testis). They are also found in the midline and make appearances in neuropathology (e.g. pineal gland) and in the mediastinum.
Overview
Germ cell tumour - types
Precusor:
Germ cell tumours (GCTs):
- Germinoma/Seminoma/Dysgerminoma.
- Yolk sac tumour (endodermal sinus tumour).
- Embryonal carcinoma.
- Choriocarcinoma.
- Teratoma.
- Mixed germ cell tumour (mixed GCT) - 60% of GCTs are mixed.
- Common combinations:
- teratoma + embryonal carcinoma + endodermal sinus tumour (yolk sac tumour) (TEE).
- seminoma + embryonal (SE).
- embryonal + teratoma (TE).
- Common combinations:
- Gonadoblastoma.
- Polyembryoma.
Grossing
- 1 cm^2 of tumour per cm of maximal tumour dimension - guideline for testicular cancer.[1]
IHC for GCTs
ABCDs of GCTs:
- AFP - yolk sac tumour.
- Beta-hCG - choriocarcinoma.
- CD30 - embryonal carcinoma.
- D2-40 - seminoma.
Tabular summary of GCTs
| Tumour | Key feature | Microscopic | IHC | Other | Image |
|---|---|---|---|---|---|
| Intratubular germ cell neoplasia (ITGCN) | nests of small fried egg cells | large central nucleus, clear cytoplasm, squared-off nuclear membrane, nucleoli[2] |
CD117 | appearance similar to seminoma | |
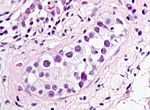
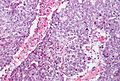
| Germinoma / Seminoma / Dysgerminoma | fried egg cells | fried egg-like cells (central nucleus, clear cytoplasm) with squared-off nuclear membrane, nucleoli, lymphocytic infiltrate, granulomata, syncytiotrophoblastic giant cells[3] |
D2-40 | seminoma = male version of this tumour; dysgerminoma = female version of this tumour | |
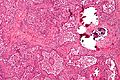
| Yolk sac tumour (endodermal sinus tumour) | Schiller-Duval bodies | Schiller-Duval b. = central blood vessel surrounded by epithelial-like cells a space and more epithelial-like cells, variable arch. | AFP | patterns: microcystic, solid, hepatoid | |
| Embryonal carcinoma | prominent nucleoli, vescicular nuclei | var. arch.: tubulopapillary, glandular, solid, embryoid bodies (ball of cells in surrounded by empty space on three sides), +/-nuclear overlap, mitoses common | CD30 | usu. part of a mixed GCT | |
| Choriocarcinoma | clear cytoplasm | cells with abundant clear cytoplasm and eccentric atypical nuclei (cytotrophoblast), very large (multinucleated) cells with abundant eosinophilic cytoplasm and extreme nuclear atypia (syncytiotrophoblast) | beta-hCG | may be preceded by a complete hydatidiform mole | |
| Teratoma, immature | primitive neuroepithelium | pseudostratified epithelium in rosettes (gland-like arrangement) | None | testicular teratomas in post-pubertal males are all considered malignant[4] | |
| Mixed germ cell tumour | NA | common combinations: teratoma + embryonal carcinoma + endodermal sinus tumour (yolk sac tumour) (TEE); seminoma + embryonal (SE); embryonal + teratoma (TE) | NA | - | |
| Gonadoblastoma | primitive germ cells (central nucleus, moderate (eosinophilic) cytoplasm); sex cord element | sex cord element may be either granulosa cells (follicle-like arch.) or Sertoli cells (trabecular arch.) | ? | often abnormal karyotype; usu. Y chromosome present |
Molecular pathology
Most common cytogenetic abnormality in GCTs:
- Isochromosome p12.[5]
- Isochromosome = one arm (p or q) is lost and replaced with a duplicate of the remaining one.
- Example: isochromosome p12 = chromosome 12 where q is lost and two p arms are present.[6]
- Isochromosome = one arm (p or q) is lost and replaced with a duplicate of the remaining one.
Germinoma
Comes in three flavours:
- Germinoma.
- Seminoma.
- Dysgerminoma.
Germinoma
Is the generic version of this tumour. It is found in the midline (brain, mediastinum).
Image: Germinoma (upmc.edu).[7]
Seminoma
A common GCT in males.
Dysgerminoma
A common GCT in females.
Yolk sac tumour
- Abbreviated YST.
- AKA endodermal sinus tumour.
General
- Rare.
- Aggressive - especially extragonadal tumours.[8]
Epidemiology:
- Most common GCT in infants and young boys.
- Bimodal age distribution:[8]
- <4 years.
- 10-30 years.
Clinical:
- Elevated AFP.
Gross
- White/yellow mucinous infiltrative mass.[9]
Microscopic
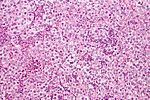
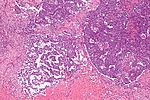
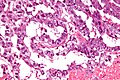
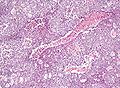
Classic feature:[9]
- Schiller-Duval bodies.
- Look like glomerulus - central blood vessel surrounded by epithelial-like cells a space and more epithelial-like cells
- Architecure - variable.
- +/-Eosinophilic hyaline globules (contain alpha-fetoprotein).
Notes:
- Has a loose stroma/vaguely discohesive -- unlike embryonal carcinoma.
- How to remember patterns REM PS GAPEH = reticular, endodermal sinus, microcystic, papillary, solid, glandular, alveolar, polyvesicular vitelline, enteric, hepatoid.
- Yolk sac tumours in adults are essentially always a component of a mixed germ cell tumour, i.e. if one sees a pure yolk sac tumour in an adult, it is probably under sampled.[12]
Variants:
- Hepatoid pattern.[13]
- Vaguely resembles liver.
- Hyaline globules (light red well-circumscribed globs).
- Bile canaculi.
- Vaguely resembles liver.
- Solid pattern.[14]
- Vaguely resembles seminoma.
DDx:
Images
www:
- Hepatoid Pattern (webpathology.com).
- Schiller-Duval body (webpathology.com).
- Hyaline globules (webpathology.com).
- Yolk sac tumour - case 1 - several images (upmc.edu).
- Yolk sac tumour - case 2 - several images (upmc.edu).
- Yolk sac tumour (moffitt.org).[15]
IHC
- AFP +ve.
- Glypican 3 +ve.
- More sensitive than AFP.[16]
- Alpha-1 AT +ve.
- Cytokeratin +ve.[citation needed]
Negative stains:[17]
- OCT3/4 - positive in seminoma and embryonal carcinoma.
- CD30 - positive in embryonal carcinoma.
Embryonal carcinoma
General
- Affects young adults.
- May be seen in women.
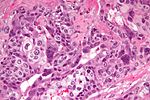
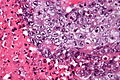
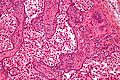
Microscopic
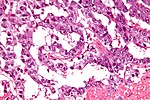
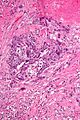
Features:[18]
- Nucleoli - key feature.
- Vesicular nuclei (clear, empty appearing nuclei) - key feature.
- Nuclei overlap.
- Necrosis - common.
- Not commonly present in seminoma.
- Indistinct cell borders
- Mitoses - common.
- Variable architecture:
- Tubulopapillary.
- Glandular.
- Solid.
- Embryoid bodies - ball of cells in surrounded by empty space on three sides.
Notes:
- Cytoplasmic staining variable (eosinophilic to basophilic).
DDx:
Images
IHC
- AE1/AE3 +ve.
- CD30 +ve.
Choriocarcinoma
General
- Aggressive clinical course.
- Usually a mixed tumour, i.e. pure choriocarcinoma is rare, e.g. dysgerminoma + choriocarcinoma.
Clinical
- High beta-hCG -- usually > 10,000 IU.
- Vaginal bleeding.
- Occasionally thyrotoxicosis.[19]
Epidemiology
- May be preceded by a complete hydatidiform mole.[20]
- More common in the far east.
- More common at extremes of fertile age (teens and 40-50 years).
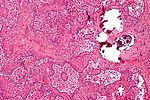
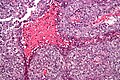
Microscopic
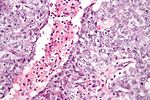
Features:
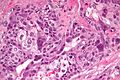
- Two cell populations:
- Cytotrophoblasts - key feature.
- Clear cytoplasm.
- Polygonal shaped cells in cords/masses.
- Distinct cell borders.
- Single uniform nucleus.
- Syncytiotrophoblasts - may be absent.[21]
- Large + many irreg. or lobular hyperchromatic nuclei.
- Eosinophilic vacuolated cytoplasm (contains hCG).
- +/-Hemorrhage - classically in the centre of the lesion.
- +/-Necrosis.
Notes:
- No chorionic villi should be present.
- If chorionic villi are present... it is likely a type of hydatidiform mole.
- The dual cell population may not be evident at first.
- Hemorrhage and marked nuclear pleomorphism are suggestive of the diagnosis.
DDx:
Images
www:
- Choriocarcinoma - low mag. (webpathology.com).
- Choriocarcinoma (webpathology.com).
- Choriocarcinoma (webpathology.com).
- Choriocarcinoma (chestjournal.chestpubs.org).[22]
- Choriocarcinoma - uterus (med.jhmi.edu).
IHC
- Beta-hCG +ve.
- MUC-4 +ve.[25]
- Ki-67 +ve -- typically >30%.
Teratoma
General
- May be benign or malignant.
- Are supposed to consists of all three germ layers - this is not always true.
- May be associated with sacral agenesis.[26]
Important note:
- The site of the tumour, age and sex are very important for predicting the behaviour of a teratoma:[27]
- Immature teratomas may have a benign or malignant behaviour.
- Mature teratomas may have a benign or malignant behaviour.
Classification
- Mature.
- Common in females.
- Usually benign.
- Mature component may give rise to a malignancy like elsewhere in the body.
- Most common malignancy arising from a mature teratoma: squamous cell carcinoma.
- Immature.
- Uncommon.
- Often malignant.
- Monodermal.
- Rare.
- Highly specialized.
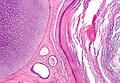
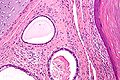
Mature teratoma
Features - three germ cell layers (usually):[28]
- Endoderm:
- Skin, (mature) CNS.
- Mesoderm:
- Muscle, bone, connective tissue, blood.
- Ectoderm:
- Internal organs.
Note:
- May consist of skin only - in which case it is commonly called a dermoid.
Images
Fetus in fetu
- Grouped with mature teratoma, as it is considered a well-developed mature teratoma.[29][30]
- It has been suggested they are distinct from teratomas.[31]
- They could be thought of as a parasitic twin.
- It has been suggested they are distinct from teratomas.[31]
Features:
- Discrete mass consisting of mature tissues that form well-developed structures with the normal anatomical relations.
- Separated from teratoma by the presence of a vertebral column.[32]
Immature teratoma
Features:
- Immature if neural tissue is present:[33]
- Vaguely resembles pseudostratified respiratory epithelium.
- Islands of small hyperchromatic cells - "blastema".
- +/-Cartilage.
- +/-Adipocytes.
- +/-Colonic type mucosa.
- +/-Stratified squamous epithelium (skin).
DDx:[34]
Images
Other images:
- Immature teratoma - myxomatous stroma (webpathology.com).
- Immature teratoma - blastema (webpathology.com).
- Immature teratoma - primitive neuroepithelium (webpathology.com).
- Immature teratoma - primitive neuroepithelium (ouhsc.edu).
Grading (immature)
Based on quantity of immature neuroepithelium:[35][36][37]
- G0 - mature teratoma; no immature neuroepithelium.
- G1 - less than one lower power field (LPF) of immature neuroepithelium; LPF defined field at 4X magnification.
- G2 - 1-3 LPFs.
- G3 - more than 3 LPFs.
Note:
- LPF not adequately defined - see LPFitis. Same BS as HPF.
IHC (immature)
Features:
- Primitive neuroepithelium:[38]
- Neuron-specific enolase (NSE) +ve.
- Neuron-specific B tubulin +ve.
- Synaptophysin +ve.
Monodermal teratomas
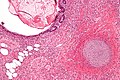
Struma ovarii
Features:
- Thyroid tissue present - colloid is seen.
- May develop pathologies seen in the thyroid gland, e.g. papillary thyroid carcinoma.
Images
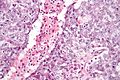
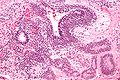
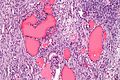
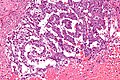
Strumal carcinoid
- Has components that suggest:
- Carcinoid (neuroendocrine tumour).
- Nuclei with stippled chromatin (salt-and-pepper chromatin).
- Thyroid - cystic spaces/follicular-like structures.
- Carcinoid (neuroendocrine tumour).
Images
Sign out
Mature teratoma
CYST ("DERMOID"), RIGHT OVARY, CYSTECTOMY:
- MATURE CYSTIC TERATOMA.
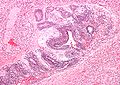
Gonadoblastoma
General
- Associated with abnormal sexual development.
- Often coexist with a dysgerminoma.
- A mixed tumour that consists of (1) primitive germ cells and (2) sex cord elements.
Gross
- +/-Cystic.
Microscopic
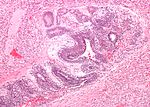
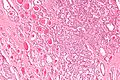
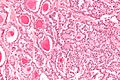
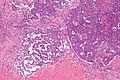
Features:[41]
- Immature germ cells resembling Sertoli cells or granulosa cells.
- Sertoli cells = moderate cytoplasm in a trabecular or tubular architecture.
- Granulosa cells = form follicle-like structures.
- May form nests.
- Primitive germ cells resemble those of a dysgerminoma.
- Polygonal cells with a central nucleus, squared-off nuclear membrane and clear cytoplasm.
- +/-Calcification (very common).
- +/-Eosinophilic basement membrane material between the (primitive) germ cells and support cells.[42]
Images
www:
- Gonadoblastoma - low mag. (webpathology.com).
- Gonadoblastoma - high mag. (webpathology.com).
- Gonadoblastoma - high mag. (webpathology.com).
- Gonadoblastoma - low mag. (flickr.com).
- Gonadoblastoma - intermed. mag. (flickr.com).
- Gonadoblastoma - high mag. (flickr.com).
- Gonadoblastoma - several cases (upmc.edu).
Polyembryoma
General
- Poor prognosis.
- Almost never in pure form, i.e. usu. a component of a mixed germ cell tumour.[43]
Microscopic
Features:
- Disc shaped structure (embryo-like) with:
- The one side endoderm.
- Skin/CNS.
- The other side ectoderm.
- Internal organs - GI tract.
- The one side endoderm.
Images:
Mixed germ cell tumour
General
- 60% of GCTs are mixed.
Common combinations:
- Teratoma + embryonal carcinoma + endodermal sinus tumour (yolk sac tumour) (TEE).
- Seminoma + embryonal (SE).
- Teratoma + embryonal +(TE).
Memory device: TEE + all combinations have embryonal carcinoma.
Microscopic
Features:
- Depends on components.
Notes:
- If one cannot identify the component... it is probably yolk sac as this has so many different patterns.
Images
www:
- Mixed germ cell tumour - several images (upmc.edu).
- Mixed germ cell tumour - several cases (upmc.edu).
IHC
- Beta-hCG +ve - if syncytiotrophoblasts are present.
- AFP +ve - a yolk sac tumour component is present.
- GFAP +ve - if neuroepithelium is present.
See also
References
- ↑ URL: http://www.uroweb.org/gls/pdf/10_Testicular_Cancer.pdf. Accessed on: 30 October 2012.
- ↑ Zhou, Ming; Magi-Galluzzi, Cristina (2006). Genitourinary Pathology: A Volume in Foundations in Diagnostic Pathology Series (1st ed.). Churchill Livingstone. pp. 538. ISBN 978-0443066771.
- ↑ Zhou, Ming; Magi-Galluzzi, Cristina (2006). Genitourinary Pathology: A Volume in Foundations in Diagnostic Pathology Series (1st ed.). Churchill Livingstone. pp. 542. ISBN 978-0443066771.
- ↑ Carver, BS.; Al-Ahmadie, H.; Sheinfeld, J. (May 2007). "Adult and pediatric testicular teratoma.". Urol Clin North Am 34 (2): 245-51; abstract x. doi:10.1016/j.ucl.2007.02.013. PMID 17484929.
- ↑ Looijenga, LH.; Oosterhuis, JW. (May 1999). "Pathogenesis of testicular germ cell tumours.". Rev Reprod 4 (2): 90-100. PMID 10357096.
- ↑ URL: http://ghr.nlm.nih.gov/handbook/illustrations/isochromosomes. Accessed on: 15 February 2012.
- ↑ URL: http://path.upmc.edu/cases/case525.html. Accessed on: 25 January 2012.
- ↑ 8.0 8.1 Shah, JP.; Kumar, S.; Bryant, CS.; Ali-Fehmi, R.; Malone, JM.; Deppe, G.; Morris, RT. (Dec 2008). "A population-based analysis of 788 cases of yolk sac tumors: A comparison of males and females.". Int J Cancer 123 (11): 2671-5. doi:10.1002/ijc.23792. PMID 18767035.
- ↑ 9.0 9.1 Mitchell, Richard; Kumar, Vinay; Fausto, Nelson; Abbas, Abul K.; Aster, Jon (2011). Pocket Companion to Robbins & Cotran Pathologic Basis of Disease (8th ed.). Elsevier Saunders. pp. 510. ISBN 978-1416054542.
- ↑ Humphrey, Peter A; Dehner, Louis P; Pfeifer, John D (2008). The Washington Manual of Surgical Pathology (1st ed.). Lippincott Williams & Wilkins. pp. 369. ISBN 978-0781765275.
- ↑ URL: http://webpathology.com/image.asp?case=34&n=1. Accessed on: March 8, 2010.
- ↑ Talerman, A. (Jul 1975). "The incidence of yolk sac tumor (endodermal sinus tumor) elements in germ cell tumors of the testis in adults.". Cancer 36 (1): 211-5. PMID 1203848.
- ↑ URL: http://webpathology.com/image.asp?case=34&n=6. Accessed on: March 8, 2010.
- ↑ URL: http://webpathology.com/image.asp?case=34&n=8. Accessed on: March 8, 2010.
- ↑ Sesterhenn, IA.; Davis, CJ.. "Pathology of germ cell tumors of the testis.". Cancer Control 11 (6): 374-87. PMID 15625525.
- ↑ Emerson, RE.; Ulbright, TM. (Jun 2010). "Intratubular germ cell neoplasia of the testis and its associated cancers: the use of novel biomarkers.". Pathology 42 (4): 344-55. doi:10.3109/00313021003767355. PMID 20438407.
- ↑ Gopalan, A.; Dhall, D.; Olgac, S.; Fine, SW.; Korkola, JE.; Houldsworth, J.; Chaganti, RS.; Bosl, GJ. et al. (Aug 2009). "Testicular mixed germ cell tumors: a morphological and immunohistochemical study using stem cell markers, OCT3/4, SOX2 and GDF3, with emphasis on morphologically difficult-to-classify areas.". Mod Pathol 22 (8): 1066-74. doi:10.1038/modpathol.2009.66. PMID 19396148.
- ↑ Zhou, Ming; Magi-Galluzzi, Cristina (2006). Genitourinary Pathology: A Volume in Foundations in Diagnostic Pathology Series (1st ed.). Churchill Livingstone. pp. 549. ISBN 978-0443066771.
- ↑ O'Reilly, S.; Lyons, DJ.; Harrison, M.; Gaffney, E.; Cullen, M.; Clancy, L.. "Thyrotoxicosis induced by choriocarcinoma a report of two cases.". Ir Med J 86 (4): 124, 127. PMID 8395487.
- ↑ Cotran, Ramzi S.; Kumar, Vinay; Fausto, Nelson; Nelso Fausto; Robbins, Stanley L.; Abbas, Abul K. (2005). Robbins and Cotran pathologic basis of disease (7th ed.). St. Louis, Mo: Elsevier Saunders. pp. 1110-1111. ISBN 0-7216-0187-1.
- ↑ URL: http://www.webpathology.com/image.asp?n=4&Case=36. Accessed on: 8 February 2011.
- ↑ Venkatram, S.; Muppuri, S.; Niazi, M.; Fuentes, GD. (Jul 2010). "A 24-year-old pregnant patient with diffuse alveolar hemorrhage.". Chest 138 (1): 220-3. doi:10.1378/chest.09-2688. PMID 20605823.
- ↑ 23.0 23.1 Cole, LA. (2010). "Biological functions of hCG and hCG-related molecules.". Reprod Biol Endocrinol 8: 102. doi:10.1186/1477-7827-8-102. PMC 2936313. PMID 20735820. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2936313/.
- ↑ Kovalevskaya, G.; Genbacev, O.; Fisher, SJ.; Caceres, E.; O'Connor, JF. (Aug 2002). "Trophoblast origin of hCG isoforms: cytotrophoblasts are the primary source of choriocarcinoma-like hCG.". Mol Cell Endocrinol 194 (1-2): 147-55. PMID 12242037.
- ↑ Mao, TL.; Kurman, RJ.; Huang, CC.; Lin, MC.; Shih, IeM. (Nov 2007). "Immunohistochemistry of choriocarcinoma: an aid in differential diagnosis and in elucidating pathogenesis.". Am J Surg Pathol 31 (11): 1726-32. doi:10.1097/PAS.0b013e318058a529. PMID 18059230.
- ↑ Online 'Mendelian Inheritance in Man' (OMIM) 176450
- ↑ URL: http://www.cap.org/apps/docs/committees/cancer/cancer_protocols/2011/GermCell_11protocol.pdf. Accessed on: 29 April 2012.
- ↑ Moore, Keith L.; Persaud, T.V.N. (2002). The Developing Human: Clinically Oriented Embryology (7th ed.). Saunders. pp. 83. ISBN 978-0721694122.
- ↑ Heifetz, SA.; Alrabeeah, A.; Brown, BS.; Lau, H. (1988). "Fetus in fetu: a fetiform teratoma.". Pediatr Pathol 8 (2): 215-26. PMID 3045784.
- ↑ Basu, A.; Jagdish, S.; Iyengar, KR.; Basu, D. (Oct 2006). "Fetus in fetu or differentiated teratomas?". Indian J Pathol Microbiol 49 (4): 563-5. PMID 17183856.
- ↑ Basu, A.; Jagdish, S.; Iyengar, KR.; Basu, D. (Oct 2006). "Fetus in fetu or differentiated teratomas?". Indian J Pathol Microbiol 49 (4): 563-5. PMID 17183856.
- ↑ Majhi, AK.; Saha, K.; Karmakar, M.; Sinha Karmakar, K.; Sen, A.; Das, S. (2007). "Fetus in fetu--a mystery in medicine.". ScientificWorldJournal 7: 252-7. doi:10.1100/tsw.2007.56. PMID 17334616.
- ↑ RS. 2 May 2010.
- ↑ Taxy, J.; Husain, A; Montag, A. (2009). Biopsy Interpretation: The Frozen Section (1st ed.). Lippincott Williams & Wilkins. pp. 34. ISBN 978-0781767798.
- ↑ Harms D, Zahn S, Göbel U, Schneider DT (2006). "Pathology and molecular biology of teratomas in childhood and adolescence". Klin Padiatr 218 (6): 296–302. doi:10.1055/s-2006-942271. PMID 17080330.
- ↑ Ulbright TM (February 2005). "Germ cell tumors of the gonads: a selective review emphasizing problems in differential diagnosis, newly appreciated, and controversial issues". Mod. Pathol. 18 Suppl 2: S61–79. doi:10.1038/modpathol.3800310. PMID 15761467. http://www.nature.com/modpathol/journal/v18/n2s/full/3800310a.html.
- ↑ O'Connor DM, Norris HJ (October 1994). "The influence of grade on the outcome of stage I ovarian immature (malignant) teratomas and the reproducibility of grading". Int. J. Gynecol. Pathol. 13 (4): 283–9. PMID 7814189.
- ↑ Craver RD, Lipscomb JT, Suskind D, Velez MC (October 2001). "Malignant teratoma of the thyroid with primitive neuroepithelial and mesenchymal sarcomatous components". Ann Diagn Pathol 5 (5): 285–92. doi:10.1053/adpa.2001.27918. PMID 11598856.
- ↑ Gorin, I.; Sastre-Garau, X. (Jun 2008). "Strumal carcinoid tumor of the ovary.". J Clin Oncol 26 (16): 2780-1. doi:10.1200/JCO.2008.16.1620. PMID 18509188.
- ↑ Tamsen, A.; Mazur, MT. (Feb 1992). "Ovarian strumal carcinoid in association with multiple endocrine neoplasia, type IIA.". Arch Pathol Lab Med 116 (2): 200-3. PMID 1346363.
- ↑ Cotran, Ramzi S.; Kumar, Vinay; Fausto, Nelson; Nelso Fausto; Robbins, Stanley L.; Abbas, Abul K. (2005). Robbins and Cotran pathologic basis of disease (7th ed.). St. Louis, Mo: Elsevier Saunders. pp. 1104. ISBN 0-7216-0187-1.
- ↑ URL: http://www.flickr.com/photos/ckrishnan/3972432044/in/photostream/. Accessed on: 11 September 2011.
- ↑ Young, RH. (Apr 2008). "Testicular tumors--some new and a few perennial problems.". Arch Pathol Lab Med 132 (4): 548-64. doi:10.1043/1543-2165(2008)132[548:TTNAAF]2.0.CO;2. PMID 18384207.